Febuary 2023 - Anushka Irodi (2020), Pembroke Medical Student
Anushka Irodi (2020) says that we should be optimistic about the Future of Health. But the NHS will need to deescalate conflicts and concede ground, or risk haemorrhaging it's workforce to sectors where they are fairly rewarded for their skills.
At a recent talk given at Pembroke by Lord Simon Stevens, former Chief Executive of the NHS, Lord Stevens was realistic about the problems the NHS is facing, but optimistic about its future. Anushka Irodi (2020), third-year Pembroke medical student, offers some poignant reflections based on some of Lord Stevens talking points, and on some of her own experiences training and working within the NHS.
The Future of the NHS
Established in 1948 as part of the post-war reconstruction effort, the National Health Service is the jewel of the UK’s welfare state. In light of all the pressure this system has been put under, both through the last decade of austerity and during the pandemic, the question posed to us: ‘What is the future of health?’ struck me as a particularly pertinent one to ask now. Earlier this month, the Master’s Seminar likewise tackled this question and asked, ‘What is the future of the NHS?’ Given by Lord Simon Stevens, the Chief Executive of the NHS until 2021, it was a thought-provoking discussion that encouraged me to think about both the advances and the challenges that lie ahead for modern healthcare.
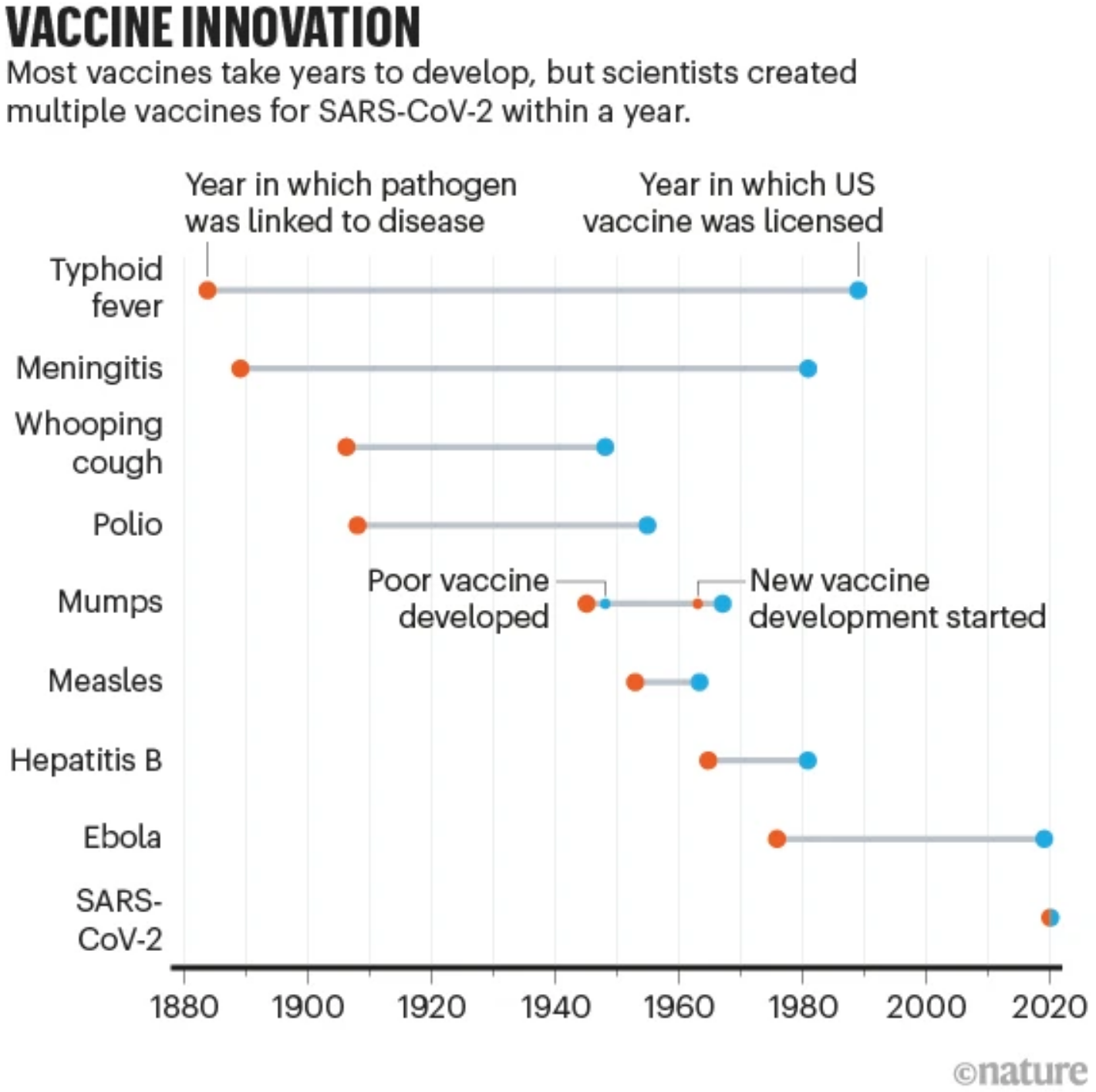
It is bolstering to reflect on and celebrate the achievements in medical science. Science is progressing exponentially faster than ever before into a new era of rapid globalised research, with millions of publications being produced each year by labs all around the world. This rich global collaborative network is highly conducive to reliable discoveries that can be translated faster into healthcare. We saw evidence of this clearly during the COVID-19 pandemic where multiple vaccines were developed at unprecedented speeds and made available on the market in less than a year!
Figure 1: Vaccine Innovation (Ball, Nature 2021)
Reference:
Ball P. Nature 589, 16-18 (2021). Vaccine Innovation [Infographic]. doi: https://doi.org/10.1038/d41586-020-03626-1
Moreover, our overall understanding of mechanisms and prevention of disease has substantially improved over the course of the last century. This is reflected in the clear gains in life expectancy as a result of public health improvements and consequent infectious disease reductions. The culmination of this approach was celebrated in 1980 when the devastating infectious disease, smallpox, was declared eradicated. Now, we enter a new frontier of healthcare with genetic testing and molecular disease characterisation informing the type of treatments that patients receive. It is a world where personalised medicine is closer than ever and the growth and input of fields such as neuroethics, which aim to address the new moral dilemmas that new medical techniques will raise, is vital.
Despite this wealth of potential that medical advancement promises, our healthcare system lies in a precarious state; the statistics of A&E waiting times, staff shortages and limited healthcare funding reflected in the media spell this out clearly. The problems that have pushed healthcare to this point are part of the public policy domain, rather than the scientific – and they must be addressed. Soon.
It is no secret that the NHS is underfunded and has been chronically so for at least a decade. This reduced spending on health manifests itself in the form of poorer infrastructure and reduced staffing and as a result, the gap between healthcare capacity and demand only continues to grow. The staff that run the NHS are its lifeblood. Yet, the same doctors that take nerve-racking life-or-death decisions on a daily basis regularly work long hours at rates of £14/hour with little scope for a healthy work-life balance. Likewise, the same nurses that care for people at their most vulnerable are left with no option but to strike when faced with pay levels that leave them incapable of financing their bills.
"There is no other profession in which this situation would be even remotely conceivable."
At a talk surrounding the ethics and efficacy of healthcare strikes last month at the School of Clinical Medicine, I listened as a liaison for a medical trade union explained how a nurse had approached him in tears after not being paid for the third month in a row. When she had asked her manager about this, she was told to focus on her patients and her work rather than her pay. There is no other profession in which this situation would be even remotely conceivable. Whilst relying on the goodwill of the profession may stave off problems in the short run, the effects will inevitably be felt in the form of severe staffing shortages as many leave to other jobs or places that will value their hard-won skills and afford them compensation accordingly. Depressingly, this will only increase the pressure on existing staff, further raising workloads and increasing waiting times, exacerbating the perpetuation of a vicious cycle.
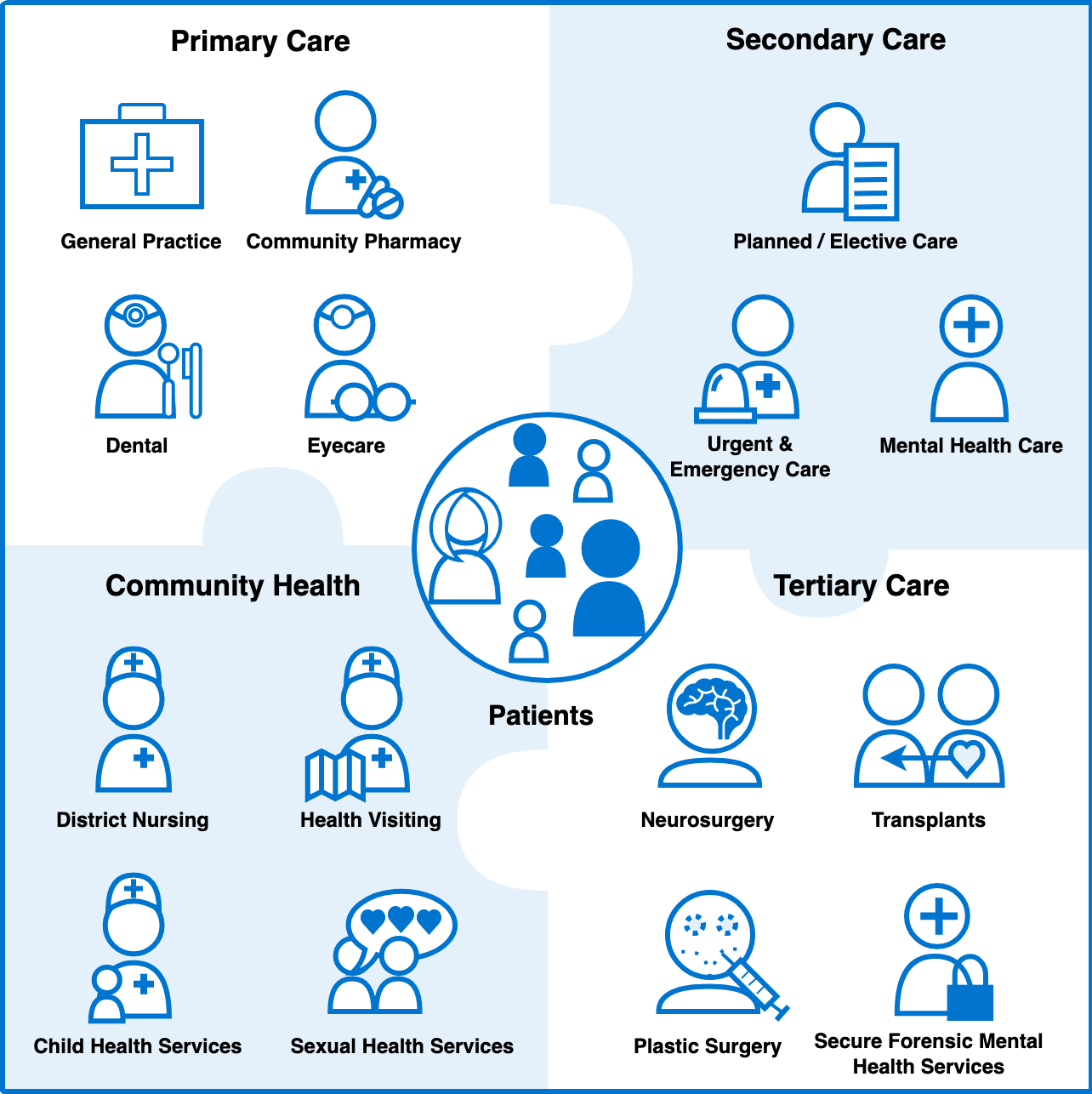
Infrastructure plays a similarly important role. Hospitals, beds and equipment all need to be scaled up to match the increased demand that naturally develops as the population continues to grow and age. Additionally, it is not just in hospital settings that improvements must be made, but also in other areas such as primary and community care. ‘Bed-blocking’ is a now notorious term that refers to situations where hospital beds are occupied by patients who do not require them but cannot be discharged due to other reasons such as lack of community or social care. As Lord Stevens explained elegantly during his talk, it is Amdahl’s law at work here – the overall performance improvement of the system will depend on the improvement of the limiting factor within this system.
Figure 2: The healthcare ecosystem (NHS, 2022)
Reference:
National Health Service. (2022). The healthcare ecosystem [Infographic]. https://digital.nhs.uk/developer/guides-and-documentation/introduction-to-healthcare-technology/the-healthcare-ecosystem
It is clear that there are multiple layers of pressure upon our healthcare system, but there is cause also for optimism. The challenges discussed here are not insurmountable but will require careful consideration and management. As a medical student, healthcare is my future. However, for all of us, our personal health is a vital aspect of our future. So we should all continue to ask: “What is the future of health?” and perhaps, “How can we protect it?”
Anushka Irodi (2020) is a third-year medical student at Pembroke currently studying Neuroscience in the Department of PDN (Physiology, Development and Neuroscience) for her intercalation. She is Co-President of the Pembroke Medical & Veterinary Society (PCMVS), Member of General Committee of the Cambridge University Students’ Clinical Research Society (CUSCRS) and has a keen interest in translational research and clinical academia. She is ever eager to try new things and has dabbled in a number of hobbies in the past ranging from Ballroom and Latin dancing to Japanese Jiu-Jitsu. She particularly enjoys music and has performed as a singer at the annual May Balls in Cambridge.