September 2023 - Rav Seeruthun, William Pitt Fellow and Founder of health-equity.ai
In communities that are marginal and being excluded from the progress being made in healthcare, AI could help to provide solutions to endemic health inequality and help to increase living standards for all.
For our September blog Dr Rav Seeruthun, William Pitt Fellow, Founder of health-equity.ai, and William Pitt Seminar speaker, tells us about the work that his latest venture has been undertaking in the fight against health inequality.
To hear more from Rav you can join us at the William Pitt Seminar on Friday 13th October. Find out more here.
How can AI help to level the field in Healthcare?
Health equity is a pressing issue in the United Kingdom that demands urgent attention and action. Despite being one of the wealthiest nations globally, the UK continues to grapple with stark health inequalities. These disparities are evident across various dimensions, including age, income, education, geography, and race. Such inequalities not only undermine the fundamental principles of fairness and justice but also result in avoidable suffering and loss of life. Addressing health equity is essential because it directly affects the well-being of individuals and communities. When certain groups experience poorer health outcomes due to factors beyond their control, it hinders their ability to lead fulfilling lives, achieve their full potential, and contribute to society. Moreover, health inequalities place an immense burden on the healthcare system and the economy as a whole, as they lead to increased healthcare costs and reduced workforce productivity. Thus, promoting health equity in the UK is not just a moral imperative but also an economic and societal imperative that will benefit the entire nation by creating a fairer and healthier society for all.
Studies have consistently shown that individuals from Black, Asian, and minority ethnic (BAME) backgrounds in the UK are more likely to experience poverty, unemployment, and inadequate housing. These socioeconomic factors directly impact health outcomes, as individuals from disadvantaged backgrounds often have limited access to healthcare services and may delay seeking medical attention. Consequently, these disparities in social determinants of health contribute to disparities in health outcomes, with BAME communities facing higher rates of chronic diseases, such as diabetes and cardiovascular diseases.
Health equity is front page news in the US. Having spent the last three years working for Genentech in San Francisco our teams were actively finding solutions to challenge health inequalities. This was an urgent issue for our patients. Whilst attending the largest oncology meeting in the world, ASCO an annual conference held in Chicago, I was shocked to discover that life expectancy from cancer can differ by up to 20 years depending on your Chicago ZIP code.
On returning to the UK, I discovered that the same was true here, there are over 50% more cases and 40% more deaths from certain types of cancer depending on your postcode. Unlike in the US though the topic of health equity is often not discussed.
"... disparities in social determinants of health contribute to disparities in health outcomes, with BAME communities facing higher rates of chronic diseases, such as diabetes and cardiovascular diseases."
How could I be part of the solution? This is where the strength of the Cambridge ecosystem became evident. The William Pitt Fellowship enabled me to have many creative and solution focussed discussions with colleagues at Pembroke. This led to further conversations with peers at Judge Business School.
I first met Professor Ian Colwill in 2013 whilst studying at Cambridge University on the Executive MBA programme. Ian is the founder of Catalyst Corporation, using AI to create solutions for the UK Ministry of Defence. My background is in healthcare, having practised as a GP in Kent, then moving on to a successful career in the Pharmaceutical Industry. Over dinner at Pembroke, we discussed our shared interest of using the power of AI to uncover unfairness in access to healthcare and innovative medicines. We decided to form a company to address these issues, health-equity.ai. Our mission at HE.AI is to detect health inequalities, to make them visible and to partner with the right people to solve them. Key partners include NHS colleagues, patient groups, politicians, diagnostic and pharmaceutical companies.
Often though to make this tangible a specific case example is needed.
The HE.AI Case for Change
Are health inequalities an issue in Diabetes management?
Diabetes is rapidly becoming a global pandemic, largely due to increasing rates of obesity. It is estimated that by 2030, diabetes will impact ~5·5 million individuals in the United Kingdom (UK), with type 2 diabetes (T2D) accounting for ~90% of all cases (ref 1).
Health inequalities and racial disparities in the United Kingdom pose a significant challenge for diabetes patients, highlighting a critical area of concern within the healthcare system.
Firstly, health inequalities manifest in unequal access to healthcare resources, leading to disparities in diabetes prevention, diagnosis, and management. Individuals from lower socioeconomic backgrounds often face barriers to accessing quality healthcare, including limited access to healthy food options and physical activity resources, which are essential for diabetes prevention and management. This exacerbates the risk of developing diabetes and makes it harder for those already diagnosed to manage their condition effectively.
Additionally, individuals living in deprived areas are more likely to experience higher rates of diabetes-related complications, such as cardiovascular disease and kidney problems, further perpetuating health disparities.
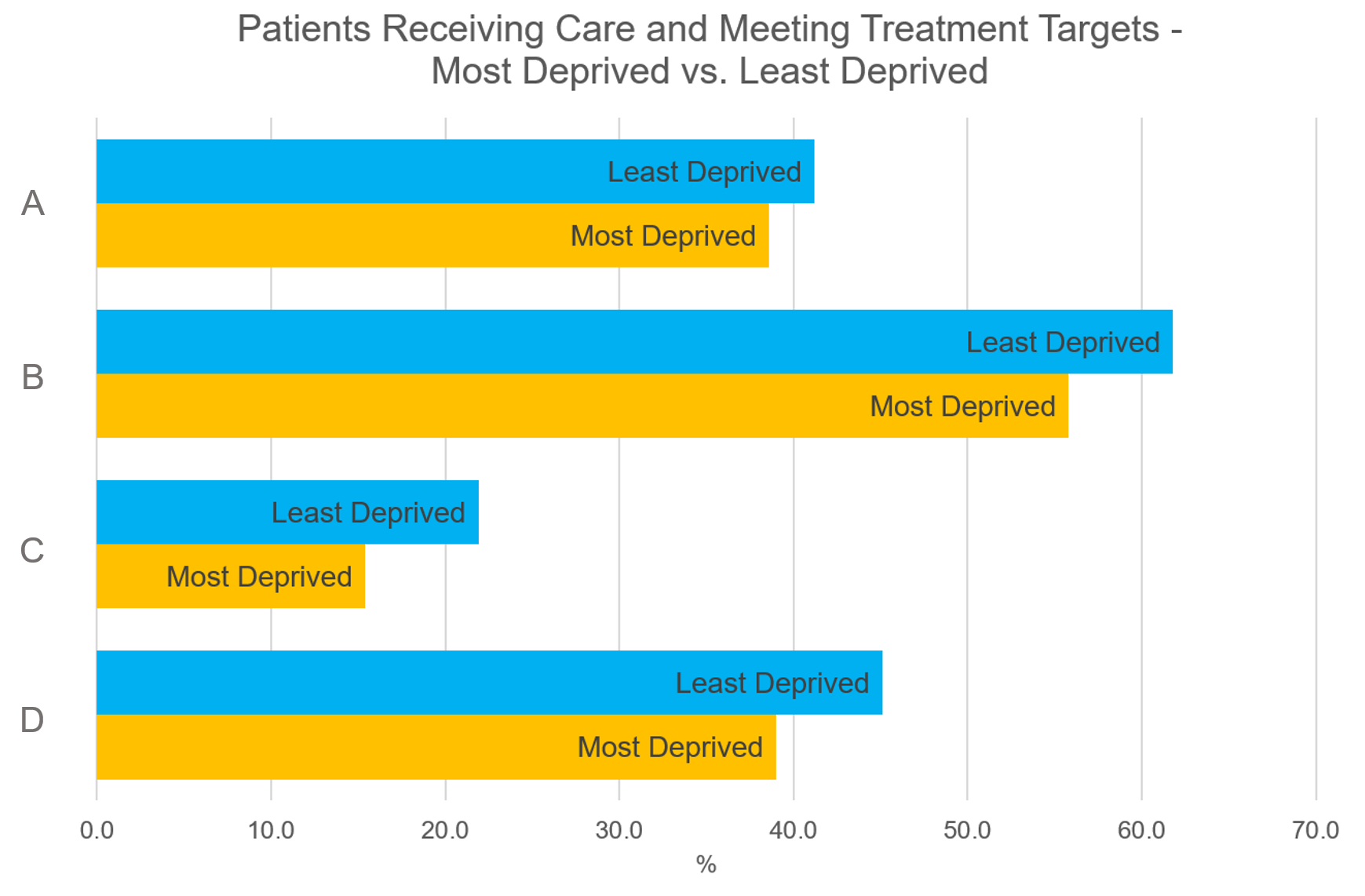
A = Type 2 patients meeting treatment targets of HbA1c, blood pressure, and cholesterol
B = Type 2 patients received all eight care processes*
C = Type 1 patients meeting treatment targets of HbA1c, blood pressure, and cholesterol
D = Type 1 patients received all eight care processes
*Body mass index, blood pressure, HbA1c measurement, cholesterol management, smoking status, foot exam, albumin:creatine ratio, serum creatine measurement
Figure 1 – Variability in Diabetes Management Related to Deprivation (ref 2)
It is well known that there is considerable variation in the delivery of diabetes care processes, structured education on diabetes, uptake of diabetes technologies and achievement of diabetes-related targets. This variability extends beyond geographic area, with inequalities also reflected across age, gender and level of social deprivation. Those in the most deprived quintile are less likely to receive all eight care processes recommended by the National Institute for Health and Care Excellence (NICE) (than those in the least deprived quintile [type 1 diabetes (T1D) 39.0 vs. 45.1%; T2D 55.8 vs. 61.8%] or to meet all three treatment targets of glycated haemoglobin (HbA1c), blood pressure and cholesterol (ref 2)
Racial disparities compound the issue, with people from Black, Asian, and Minority Ethnic (BAME) communities in the UK disproportionately affected by diabetes. Several factors contribute to this, including genetic predispositions, cultural differences in diet and lifestyle, and unequal access to healthcare. Language barriers, discrimination, and mistrust of the healthcare system can also hinder diabetes patients from BAME backgrounds in seeking timely and appropriate care. Addressing these disparities requires a multifaceted approach that involves culturally sensitive healthcare services, targeted outreach and education programs, and policies aimed at reducing socioeconomic inequalities to ensure that all individuals, regardless of their racial or ethnic background, have equal access to the resources needed for effective diabetes management and prevention.
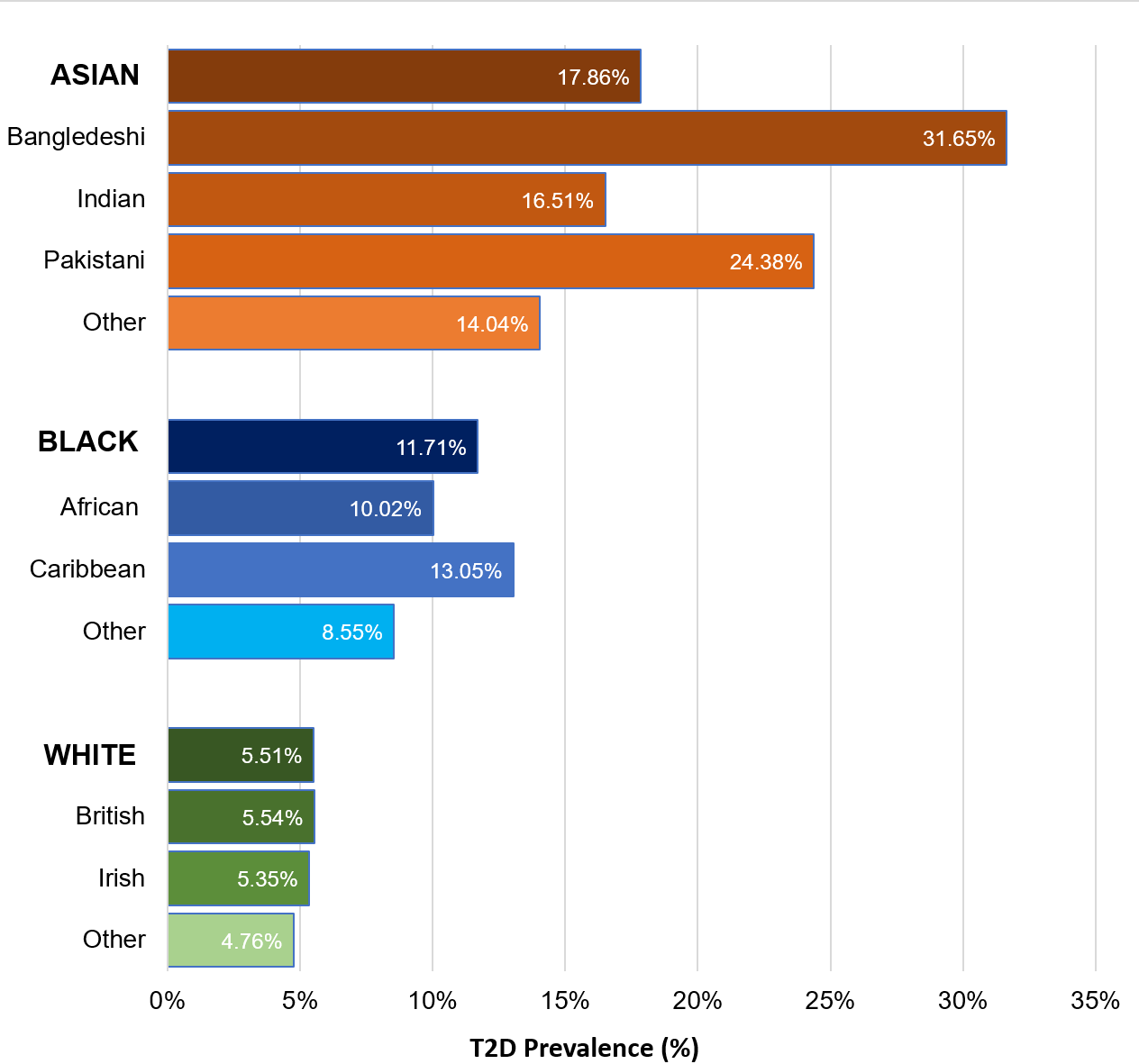
T2D is a health disparity that disproportionately impacts minority ethnic groups. Asian and Black ethnic groups in the UK have approximately two to four times the T2D prevalence compared to White and other ethnic groups.
T2D Prevalence by Race
Figure 2 – T2D Prevalence by Race (ref 3)
A systematic review of 51 studies, mainly conducted in the USA and UK, reported that overall people with diabetes from ethnic minorities have higher mortality and morbidity rates (ref 3)
Finally, age is not often discussed as a health equity issue. Analyses have shown a significant cross-sectional association between perceived age discrimination in two or more situations and diabetes (ref 4). With the advent of newer Continuous Glucose Monitoring technologies, where you constantly track your blood sugar measurement, with the associated use of your phone and Apps we strongly believe this is an area where we should address the potential for digital exclusion in older people.
How are we part of the solution? We are currently deploying our AI-driven analytics to identify specific areas of the UK where action needs to be taken and have key partners on-board to address these health inequalities.
Our Call to Action.
On March 25th, 1966, Martin Luther King said “Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane”.
57 years later, it is shocking and unfair that underserved populations do not have equal access to healthcare and innovative medicines.
As we live longer, how health equity differs with age is rarely discussed. Age is in fact estimated to be the most important determinant of health. Yet while older persons on average have greater health care needs than younger age groups, they also face distinct disadvantages in accessing appropriate, affordable and quality care.
At the 18th William Pitt Seminar in under one month, I will be joining a distinguished panel as co-founder of health-equity.ai and William Pitt Fellow to talk about health inequality in the UK at #WPS2023 join us by signing up here.
We believe that openly discussing these issues is the first step in creating actionable solutions. By ‘levelling up’ we will ensure better outcomes for more patients.
References
1. Socioeconomic deprivation and genetic ancestry interact to modify type 2 diabetes ethnic disparities in the United Kingdom, Shashwat et el. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00240-6/fulltext#bib0002
2. Social Inequality and Diabetes: A Commentary. Diabetes, Barnard-Kelly et el. https://pubmed.ncbi.nlm.nih.gov/32124269/
3. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients. Lanting LC, et al. https://pubmed.ncbi.nlm.nih.gov/16123507/
4. Associations between age discrimination and health and wellbeing: cross-sectional and prospective analysis of the English Longitudinal Study of Ageing, Jackson et el. https://www.thelancet.com/pdfs/journals/lanpub/PIIS2468-2667(19)30035-0.pdf
Dr Rav Seeruthun MD is co-founder and Chief Medical Officer at Health-Equity.AI, a company that identifies health disparities using AI and partners on the actions needed to solve them. Previous to this he served as an Officer and Vice-President at Genentech in San Francisco where he managed over 500 people in a variety of different roles across the US. He has worked in both Medical and Commercial roles including being the UK Country Medical Director and a Business Unit Director at Roche.
Rav studied medicine at Imperial College, London and practised for eight years in the NHS before joining the pharmaceutical industry in 2007. Prior to Roche, Rav worked as Senior Director of Medical Affairs at PPD, and as Head of Neurology for Eisai Europe. He also holds a Bachelor of Science degree in Psychology from University College, London and an Executive MBA from Judge Business School, Cambridge.